“Suspended Animation” Proof-of-Concept: Alcor’s Pioneering Total Body Washout Experiments
Introduction
The first stage of a human cryopreservation consists of cardiopulmonary support, heart-lung bypass, and moderate patient cooling. These measures are known to be reversible because they are successfully used in ordinary medicine. The next stage of human cryopreservation consists of replacing all blood with a “base perfusate”, cooling to near 0°C (the freezing point of water), and circulating the bloodless (asanguineous) perfusate for several hours while cryoprotectant is introduced. As of the mid-1980s, nothing like this had ever been done before, in either animals or humans.
In 1984, Alcor and Cryovita laboratoraties began a pioneering series of experiments to demonstrate that large animals (dogs) could survive up to 4 hours of “total body washout” (TBW) and maintenance at a temperature only 4°C above the freezing point of water. These successful experiments were presented at the 1985 annual meeting of the Society for Cryobiology.
Unfortunately publication of the abstracts was blocked because of political opposition of the Society to cryonics. This action is documented in the June 20, 1985, minutes of the annual Board Meeting of the Society:
“The Board shall instruct the Editor-in-Chief of the Journal of Cryobiology to not publish abstracts numbered 48 and 49 submitted for presentation at the 1985 Annual Meeting of the Society for Cryobiology on the grounds that publication would be detrimental to the Society for Cryobiology.”
Further details of this unfortunate episode in the history of cryobiology, and the thinking behind it, can be found in the article Cold War: The Conflict Between Cryonicists and Cryobiologists.
In the 1990s, scientists outside of cryonics (including one who was instrumental in blocking Alcor’s publication in 1985) achieved similar results and went on to make hypothermic suspended animation a “legitimate” and recognized field of medical research. Below we present an anthology of lay-level reports published in Cryonics magazine to document for the historical record that cryonics scientists did it first! The unpublished scientific report of this work can be read here.
Cryonics, July 1984
NEW PERFUSATE FORMULATION
Since the early 1970’s the base perfusate used in cryonic suspensions has been undergoing a steady evolution. Initially, this evolution was directed primarily by armchair research in the form of looking at the cryobiological literature and extrapolating to our circumstances. After about 1973, cryonicists began conducting their own research to evaluate the best perfusate formula, and since 1977 we have had definite criteria for making changes, namely that changes must be shown to be a substantial improvement in terms of cost and/or ease of handling and must be at least as good or better than the preceding formulation at supporting viability. We have also required in-house tests of the perfusate’s compatibility with the cryoprotective agent currently in use. Further in-house testing is required to insure that the perfusate can be used safely in an intact animal, i.e, during perfusion. This latter requirement is to insure that a perfusate which checks out well with tissue slices be shown not to cause serious edema or other gross side-effects which might not become apparent until it is actually perfused.
All of the perfusates in use since 1974 have been “glycerophosphate- based” or in other words, have gotten a large fraction of their buffering (acid neutralizing) and/or osmotic (water holding) activity from sodium glycerophosphate, a sugar-salt. The use of glycerophosphate-based perfusates was a tremendous advance over previously used “simple” electrolyte solutions such as Ringer’s solution. Indeed, the use of glycerophosphate has in part been responsible for allowing closed circuit, cryoprotective perfusion to proceed for as long as 7 hours in ischemic human patients before edema (tissue swelling) becomes a limiting factor.
There are, however, some problems associated with the use of glycerophosphate- and phosphate-based perfusates. Recent research conducted by Buckberg, et al (1) has demonstrated the need for “high” pH (8.0 or higher) in the range of 10 to 15 degrees centigrade. Unfortunately, phosphate buffers such as those employed in a glycerophosphate-type perfusate cannot easily remain in solution at this high of a pH. The result is precipitation of these chemicals which in turn causes unstable perfusate composition and loading of filters during perfusate preparation. Also, the phosphates tend to take magnesium and calcium with them when they precipitate out of solution. Stable magnesium, calcium and phosphate levels are essential to good viability and adequate perfusion.
For these reasons, about a year ago ALCOR began experimenting with synthetic organic buffers: principally HEPES (which is short for N-2- hydroxyethyl piperazine-N’-2-ethane sulfonic acid). HEPES, unlike glycerophosphate, is compatible with high pH’s and does not cause precipitation of calcium and magnesium salts. HEPES is also compatible with good tissue viability and a formulation very similar to the one we’ve chosen to replace our glycerophosphate based perfusate is now in use at the Red Cross Blood Research Lab by investigators working on kidney preservation, with similar good results.
Our own tests in perfusing cats and rabbits with this perfusate indicate no untoward gross effects. Perfusate mixing has been greatly simplified by substitution of the HEPES and filter loading has been substantially reduced as well.
The formula we are currently using is given below:
MANNITOL-HEPES PERFUSATE FORMULATION
Dextran 40 50g/l
Mannitol 170.0mM 30.97g/l
Glucose 10.0mM 1.80g/l
HEPES 7.2mM 1.72g/l
Glutathione 5.0mM 1.54g/l
Sodium Bicarbonate 10.0mM 0.84g/l
Adenine HCl l.0mM 0.17g/l
Potassium Chloride 28.3mM 2.11g/l
Calcium Chloride l.0mM 0.5ml of 22.2% solution
Magnesium Chloride 2.0mM 1.0ml of 40.66% solution
Sodium Heparin 1,000 units/l
We print this formula as a point of information for our own members. We wish to emphasize that this does not constitute a recommendation to other cryonics organizations. Each organization should carefully evaluate perfusate formulations in-house before changing their perfusion protocol.
Cryonics, September 1984
A BRIEF OVERVIEW OF RECENT ALCOR RESEARCH
Over the past year ALCOR has been steadily gaining expertise and experience in subjecting dogs to extracorporeal circulation and deep cooling. As far back as 1979, ALCOR and Cryovita have been interested in evaluating extended bloodless support of dogs in deep hypothermia. This kind of work is crucial to being able to assess viability after cryoprotective perfusion and freezing or vitrification in the brain. Until we know we have a pretreatment, cooling and surgical protocol, as well as a perfusate formulation which is compatible with viability, we cannot begin to move on to introduction and removal of cryoprotective agents.
ALCOR, in cooperation with Cryovita, has also had the unexpected and welcomed opportunity to examine human remains which had been cryopreserved for a number of years. Within the next few months we will conclude our presentation of findings generated as a result of these studies.
On the weekend of July 21-22, we undertook another total body washout experiment, this one designed to complete evaluation of the new perfusate formulation developed for human suspensions published in the July issue of CRYONICS. This perfusate is designed to allow for extending storage (1 to 3 days) at temperatures just above the freezing point of water. Since one of our major research objectives for next few years is to develop reversible techniques of suspended animation for the central nervous system, we were anxious to find out if this perfusate would be compatible with complete recovery of the brain following blood washout and deep hypothermia.
We are pleased and proud to report that the ALCOR suspension team again delivered and we had recovery of an animal from total body washout (hematocrit between 4 and 5) and cooling to a temperature of 4.2 degrees centigrade. We are especially pleased with this success because the procedure was so technically demanding and this was our first time using this approach.
Because the perfusate employed has a composition very different from normal body fluids with respect to salt and other electrolyte content, we had to connect the animal to an artificial kidney machine and “dialyze” him as we rewarmed. This allowed for normalization of blood glucose and electrolytes. Since the animal was intended to recover in order to allow for extended evaluation of general health and mental status, we employed sterile technique. In the future, when we are working with isolated head preparations to establish brain viability, simpler and far less costly protocols can be used. Even with the use of sterile technique the total cost for the experiment was only around $1,000.
At this time the dog, whose name is “Star” (courtesy of Anna Tyeb) is fully recovered and shows no neurological or other deficits. As far as we know this is the first time anyone has succeeded in cooling a large, nonhibernating animal to a such low temperature, carrying out blood washout with a very “alien,” nonphysiologic perfusate, perfusing for one hour, and then successfully rewarming. We are quite surprised at our success as we had expected many complications and failures before the first long-term recovery.
Our success with Star, and with the other dogs we have surface cooled and perfused recently has led to increased funding support for this area of research. Over the next six months or so (time more than money permitting) we hope to complete a series of five or six animals who have been similarly treated. We will delay a full technical presentation until this work is completed, but we will keep everyone posted on the general nature and pace of our progress, as well as reporting on any unforeseen developments which may impact suspension patient care.
Cryonics, November 1984
TWO MORE TOTAL BODY WASHOUTS COMPLETED
Since we reported on our success with Star in the September issue, we have undertaken two more total body washouts, both of these with four hours of asanguineous (bloodless) perfusion at 4 degrees centigrade, again using a slightly modified version of the base perfusate designed to be employed by ALCOR in human suspensions.
The first of these two experiments ended in outstanding success with long term survival of the animals. “Enkidu” (pronounced “Inky-do”, named after the friend Gilgamesh sought to bring back from hell in “The Epic of Gilgamesh”) is a good example of what dedication can do. “Inky”, as he came to be called, required nearly a week of around the clock intensive care nursing. He did not eat his first solid food for nearly a week, and he required constant turning, suctioning, medicating and high quality supportive care day and night. Unfortunately, Jerry Leaf and Mike Darwin had to be away in the days following the experiment (they were attending the Society for Cryobiology meeting in La Jolla) and that left the job of nursing Inky back to health to Anna Tyeb and Hugh Hixon. Most of that difficult job fell to Anna, who virtually lived at the lab for a week — largely without relief — struggling to bring Inky safely back from the “dead.” Indeed, it was Anna’s suggestion that she (as well as the rest of us) had “gone through hell to bring him back to life” which suggested his name.
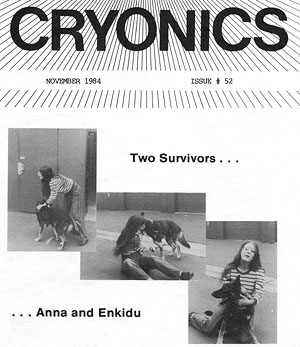
The photos on the cover show Anna with a fully recovered Inky behaving in his usual, uncontrollable way. One thing which Inky definitely demonstrated is the preservation of memory and personality after cooling to 4 degrees centigrade. Inky was unmanageable and “difficult” before the experiment, and this behavior was present after his recovery as well.
Four weeks after the experiment, Inky was sacrificed and subjected to fixative perfusion and a careful postmortem examination (including tissue histology) to check for any lingering effects of the four hours of cold asanguineous perfusion. Gross examination revealed no sign of injury. Histological examination will be completed in a month or two.
The third experiment was conducted on the weekend of the 29th of September and was also a 4 hour washout/perfusion, this time with cooling to 1 degree centigrade. After the experiment was underway, we realized that we had a very sick animal on our hands (apparently a viral intestinal infection). The intestinal infection, complicated by washout and anticoagulation degenerated into intestinal bleeding almost immediately post operatively and the animal died 12 hours after rewarming with only slight recovery of consciousness. We also noted some other problems (probably unrelated to the infection) with the pancreas and the dura (the dura mater is a tough membrane that covers the brain) which may have been a result of perfusion at so low a temperature. We are taking steps to try and avoid these problems in the future.
None of the animals demonstrated any sign of pulmonary edema and the necropsy performed on animal #3 showed the lungs to be in excellent condition. In the past, pulmonary edema has been a major stumbling block to recovery of animals after asanguineous perfusion.
We have 3 to 4 more experiments in this series planned, and we hope to have the work wrapped up by March or April of 1985.
As an aside to those who’ve asked, Star, our first TBW survivor has found a home with a family in the San Diego area and is reportedly doing very well. Star was a very special beast to all of us, and it gives everyone here at ALCOR great pleasure to know that his good natured gentleness is making other people happy.
Cryonics, December 1984
TOTAL BODY WASHOUTS: MORE PROGRESS
The ALCOR Suspension/ Research Team has completed Total Body Washout (TBW) #4. This animal, named Mr. Bear, was subjected to blood washout (hematocrit was unreadable), cooling to 5 degrees C, and four hours of continuous perfusion at that temperature. We were better able to control some of the variables which were partly responsible for failure with our last animal (namely too low a perfusion temperature, acidosis and poor electrolyte balance). Mr. Bear recovered from perfusion much faster than our previous four-hour survivor, Enkidu (see November 1984 CRYONICS). Mr. Bear was eating solid food 48 hours after perfusion and was walking within 72 hours.
Twelve days following the experiment Mr. Bear had recovered most of his previous energy level and was going for extended outdoor jaunts. One of the fascinating and rewarding things about this work is the opportunity it has afforded us to study the physiology of the post-perfusion state. By monitoring the animal’s biochemistry we have been able to track injury (and recovery) of various organ systems as a consequence of perfusion. We are very excited by the results we’ve obtained so far and hope to have more results to offer in the near future.
So far we’ve subjected four animals to TBW; three for 4 hours and one for 1 hour. We have had all these animals survive with the exception of one 4-hour animal.
The volunteers who’ve shown up weekend after weekend deserve the generous thanks and support of ALL the ALCOR membership. It is especially worth noting that Sherri Cosgrove, Jerry Leaf, Brenda Peters, Al Lopp, Scott Greene, and Hugh Hixon spent the night at Cryovita (bunked out on the floor, sofas and anywhere else that would hold them) with very little sleep and no creature comforts. It’s hard to say how good the thought of a shower, clean clothes and a warm bed can seem after 18 hours of tense activity in scrub suits! These team members avoided the lure of a quick escape and stuck it out till Mr. Bear regained consciousness. Sherri and Jerry deserve a special thanks as they remained awake for over 20 hours continuously (constituting a two person ICU nursing crew) when the rest of the team had sacked out (and Mike Darwin had snuck off to home). To all of the team: congratulations and keep up the good work!
Cryonics, February 1985
RESEARCH UPDATE
We have completed another Total Body Washout (TBW) successfully. This experiment did not go as smoothly as the others have in the post-operative phase. However, the animal survived and is doing well (see “Bringing Dixie Back” elsewhere in this issue). This marks the third successful 4-hour, bloodless perfusion at 4 degrees centigrade we have completed. As of now we have two more 4-hour perfusions scheduled before wrapping up this project.
Cryonics, March 1985
TOTAL BODY WASHOUT #6 COMPLETED
We have now completed all but one in our Total Body Washout (TBW) series and we are relieved to report that TBW-6 went smoother than any of the preceding experiments, including our one-hour perfusion, TBW-1 (Star). “Ghost,” a pure white German Shepherd who was the experimental animal, recovered at a rate comparable to that seen in dogs who had merely been placed on bypass and NOT washed out. Ghost was eating within 12 hours of the conclusion of the washout and four- hour, blood-free perfusion. He was walking and exhibiting normal energy levels within less than a week.
Thomas Donaldson, head of the Australian cryonics contingent, attended the session and was able to get his hands wet (literally in this case, since one of the things Thomas did was to fill ice bags). Thomas was also able to get a short course in some more sophisticated skills such as manual ventilation, medical packaging and drug dosages. It was also an opportunity for Thomas to “get the feel” of the clinical environment during a situation which closely parallels a cryonic suspension.
We’re not certain why Ghost recovered faster than our other TBWs, but we strongly suspect that it was a result of better regulation of perfusion pH. In the past we have had persistent problems with acidosis during the recirculation period of perfusion. After we get down to 4øC or so, perfusate pH becomes progressively more acid with pH sometimes falling as low as 6.99! Normally, this is considered a lethal pH, but we have consistently had animals recover from a pH this low. Our strategy in past experiments has been to treat the low pH by giving periodic doses of sodium bicarbonate. During our last perfusion with Dixie, our pH problems were so persistent that we decided to continuously administer intravenous sodium bicarbonate throughout the perfusion. We started this maneuver about halfway through the perfusion. Our pH was much better controlled by the slow bicarb drip than we had expected it would be.
As a consequence, with Ghost we decided to start a bicarb drip from the beginning. Much as we expected, perfusion pH was the best it had ever been: 7.56 almost from start to finish. We are excited by Ghost’s prompt recovery, and especially excited by the results of the blood concentrations of tissue enzyme we monitor as indicators of injury. Ghost had very low elevations of liver, pancreatic and other tissue enzymes compared to the previous animals.
It’s too soon to tell if better control of pH was responsible for Ghost’s improved biochemical and functional recovery. Hopefully the final experiment in our series will bear out the good results achieved with continuous buffering. If this turns out to be the case, it will be real cause for excitement since it implies that most of the injury we have been observing so far and attributing to perfusion, may really be nothing more than a failure to adequately control pH.
Cryonics, May 1985
TOTAL BODY WASHOUT # 7 — WRAPPING UP
On the weekend of March 22, we carried out the final experiment in our preliminary series of total body washouts. These experiments were designed to verify the compatibility of our “synthetic” perfusate with survival and recovery of dogs after four hours of perfusion at 4°C. As regular readers who have been following this work will know, we have had success in five out of six previous experiments in achieving long term recovery of animals. Five of the six previous TBWs involved four hours of recirculation at 4°C with one of these experiments terminating in the death of the animal 12 hours following the conclusion of the perfusion. That animal died as a result of intestinal and pancreatic bleeding (probably secondary to an undetected viral infection present before the experiment started).
It was hoped that this final experiment would allow us to apply insights gained from the previous six in a way that would allow for even more rapid recovery of this animal, with fewer of the complications and less tissue injury than had been observed in some of the earlier experiments.
Unfortunately, our expectations were thwarted, and what we thought was going to be a flawless, routine experiment turned out to be a case study in an unusual complication.
The animal we selected for the experiment was a Huskie mix whom Mike christened “Nanook.” The blood donor animal was a dog which had been previously transfused. Previously, we had not found it necessary to use dogs with a history of transfusions and we had been unaware until recently that they can be the source of hemolytic (red cell destroying) antibodies. Due to the extremely short supply of research animals on the West Coast (largely as a result of the animal rights activists) we were faced with no choice but to use this previously transfused animal as a blood donor.
The experiment, which got underway early on Saturday morning, proceeded so smoothly at the start that we completely forgot our anxieties about the donor dog. Usually, if you’re going to have a transfusion reaction you see it right away, as soon as the test dose of blood is given or the animal first goes on bypass. Bypass, cooling, and washout proceeded smoothly. We were especially pleased with the smooth progress since we had a visitor from the Bay Area, Dr. Hal Sternberg, a Ph.D. biochemist working with Paul Segall and Harry Waitz of Biophysical Research and Development on the BACS hamster perfusion project (see Bay Area Update elsewhere in this issue for details).
We tried, with a fair amount of success, to control the low pH which had plagued us pretty consistently up until the previous experiment. Al Lopp suggested continuously monitoring pH during the perfusion, and then volunteered for the job himself. Essentially what Al did was to sit at the blood gas console more or less continuously for about six hours and do perfusate and blood pH and gas determinations over and over again, constantly monitoring the progress of the animal and insuring that the pH didn’t take a nosedive while no one was watching (which it can do very quickly). During the previous experiment, about half way through dialysis we hit on the idea of continuously monitoring the pH of the dialysate (which quickly alters the blood pH to the same value) by immersing a pH electrode directly in the dialysate. We repeated this procedure during this experiment and found it very useful in providing for more or less dynamic control of pH during re-warming. Throughout the rewarming and blood re-perfusion phase of the experiment everything seemed to be going smoothly.
Our problems began to surface when the animal failed to regain consciousness when expected. (Fortunately or unfortunately, depending on your point of view, Dr. Sternberg was unable to stay for the “revival phase” of the experiment). This was disturbing enough but was soon overshadowed by developing cardiovascular collapse. The animal began experiencing a variety of cardiac arrhythmias and developing shock as evidenced by a climbing heart rate — at times well over 240 beats per minute. Despite fluid support and vasoconstricting medication, the heart rate stayed up and the animal continued to deteriorate. At 5:54 AM on Sunday Mike Darwin administered some Verapamil (a slow calcium channel blocker) in a last ditch attempt to short circuit the tachycardia (high heart rate). Shortly afterward the heart rate declined a little and stabilized. Mike went home to get some sleep (so he could relieve Jerry and the rest of the crew later in the day) and Jerry Leaf took over. Shortly after Mike left, the mystery of the tachycardia was solved. The dog voided several hundred cc’s of black urine. A hematocrit was immediately done and it was discovered that the animal had lost slightly less than 2/3rds of his red cells to hemolysis! The hematocrit had dropped from a post-pump value of 26%, to 11%! Despite the fact that this is normally a lethal hematocrit for a stressed, post-surgical animal, Nanook slowly woke up and by 12:30 PM he was sitting up briefly and lapping water.
Nevertheless, the prognosis was not good. His heart rate was still higher than could probably be sustained for long, and he would need more oxygen-carrying cells to effect convalescence and recovery. Unfortunately, on a Sunday afternoon a couple units of dog blood is not something one can run down to the grocery store and buy. With time, it might be possible to round up a unit via one of the animal emergency clinics (since they maintain bleeder animals), but the problem was where to get blood now.
Finally, it was decided to expend some of a very precious commodity which we had been holding in reserve: a unit of Fluosol-43, a Japanese fluorocarbon blood substitute which is tremendously expensive and even more tremendously difficult to come by (the two units Cryovita had were a gift from a Japanese investigator friend of Jerry Leaf’s). With a mixture of wistfulness and anticipation we administered the Fluosol-43. Within minutes of beginning the infusion of oxygen-carrying fluorocarbon micelles, Nanook’s heart rate began to drop. His energy and alertness improved immediately thereafter.
Meanwhile, Mike Darwin began some energetic searching and managed to locate a pet clinic which could spare a unit of blood (it was a busy weekend for the emergency pet clinics too! ). At 7:30 PM, a transfusion of a unit of Doberman blood was started. Nanook promptly proceeded to hemolyze about 1/3rd of the transfused cells, but following vigorous treatment with steroids and benadryl the hemolysis stopped and his hematocrit stabilized at 21%, a survivable value (and more than adequate when the contribution of the Fluosol was added in).
Nanook’s convalescence was delayed a little (though not as much as we expected) by his severe transfusion reaction. However, his recovery was complete and we are glad to report that he went home with his new “companion” today, April 8th! Nanook was fortunate enough to be adopted by Al Lopp, whose efforts no doubt in large measure contributed to his survival and reasonably prompt recovery.
A SPECIAL THANK-YOU TO CRYOVITA
The recent suspension of an ALCOR member and the recent completion of the TBW series, whose success has outdistanced our wildest expectations, bring powerfully home the need to point up the role of our “quieter” partner and to offer thanks.
Jerry Leaf, and Cryovita Laboratories of which he is president, has contributed at least as much, and being honest, maybe more, to the success we’ve experienced than our own efforts have. Frankly, we’ve been negligent by not acknowledging the role Cryovita has played in ALCOR’s development and growth. By allowing us to occupy space at Cryovita at a ridiculously low rent, and by providing, free of charge, his expertise and equipment, Jerry Leaf, more than any other man, past or present, has contributed to the growth and success of ALCOR. His faith in us and his support is genuine and motivated only by a desire to see cryonics succeed and to see the research move forward. We can’t thank Jerry and Cryovita enough.
In this series of TBW experiments Cryovita has shared with us, as an equal (and sometimes unequally burdened) partner. Credit for our success needs to be redefined: the “our” here is ALCOR and Cryovita.
In the suspension we recently completed it was Cryovita’s generosity which to a large extent allowed us to facilitate growth of our donor fund by keeping marginal costs and outside charges for perfusion to a bare minimum. While it is true that the ALCOR staff provides services and benefits (by their presence) to Cryovita, they also inflict real liabilities (you should see the utility bills these days!). In the two-way street of cooperation it has clearly been Cryovita who has been logging the heaviest mileage.
Direct ways of repaying Cryovita are hard to come by in these early days. Mostly, what we have to offer is our thanks and our promise to keep up the pace of progress and to concentrate our resources, as we have in the past, on expanding our understanding of cryonics/cryobiology. We hope to have Cryovita with us every step of the way, hopefully as a less abused partner in the future! In the meantime: THANKS! WHAT WOULD WE DO WITHOUT YOU?!
